ANATOMY AND MECHANISM
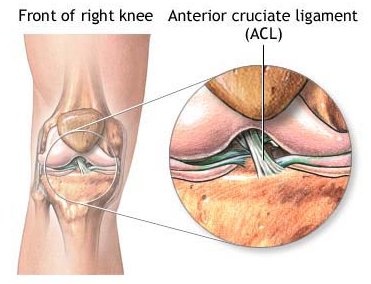
A meniscus is a C-shaped piece of cartilage that acts as a shock absorber of the knee, protecting the bones from wear and tear. There are 2 menisci in each knee joint, 1 one either side. Meniscal tears usually occur as a result of twisting movements, where the foot remains planted on the ground, and are common in sports such as volleyball, netball, basketball, soccer and rugby.
SIGNS AND SYMPTOMS
- Pain, particularly with activities that involve twisting or bending the knee
- Clicking and/or locking
- Swelling – usually 24 hours following injury
- Difficulty bending and fully straightening knee
The extent of the signs and symptoms will depend on the severity of the tear. With larger tears generally more pain is felt. Also, with certain types of tears, flaps can lift up and cause the knee to lock which is usually very painful.
TREATMENT
Immediate treatment, and within the first 3 days, consists of the RICE principles:
Rest – Rest your knee, avoid too much walking and refrain from playing sport.
Ice – Every 2 hours apply ice, this will help with the pain and swelling.
If using an ice pack (or frozen peas), leave it on for 10-20 minutes, using a tea towel or similar between the pack and skin to prevent ice burn.
If using an ice cube, “massage” your knee with the ice, gently rubbing it over the skin. Keep the ice cube moving to prevent ice burn and do this for no longer than 5 minutes.
Compression – Use Tubigrip (or a stretchy bandage) on the knee to apply some compression to the joint. This will help to alleviate swelling.
Elevation – Prop your leg up so that your knee is elevated above the level of your heart. This will help to minimise the swelling.
Initial physiotherapy treatment will include gentle joint range of motion and strength exercises aimed at preserving movement and muscle strength. It will also focus on reducing swelling, managing pain and restoring a normal walking pattern. You should do light pedalling on an exercycle with little resistance as this will keep your knee moving with minimal to no pain as it is not having to support your bodyweight.
As pain and swelling decreases your physio will progress your exercise programme, eventually introducing agility and impact exercises. The last phase of rehab will be focusing on sports-specific exercises (if the aim is return to sport).